Miswaki Village, Tanzania—When her water broke, Helena Paschal was alone at home. Although her due date was several weeks away, she knew the labor was real. “I felt a sharp pain around my waist. I sensed the baby was coming,” she recalled. There was no time to call a neighbor or do anything but just bear down and push. The baby arrived in a pool of blood. Helena gathered her strength, grabbed a nearby knife and cut the umbilical cord.
It would be the next day before her family took her and the baby to the village health dispensary. But it was too late. Tiny and weak, Helena’s baby died. The year was 2019.
Last summer, Helena found herself in much the same situation—premature labor at seven months, home alone, again. But this time, the 23-year-old, her husband and their baby made it to Miswaki Dispensary in time and were soon in the care of a petite and powerful nurse-midwife.
“Helena was very pale and weak when she arrived here that morning,” recalled Midwife Rose Julius Hamisi. “Thankfully, her 1.3 kilogram (2.9 pound) preemie baby was still alive but very weak.”
Newly assigned to Miswaki Dispensary, well-prepared and ready to take charge, Midwife Rose provided emergency care to Helena and her baby. She also taught the new mom and her husband how to provide kangaroo care, a low-cost, highly effective series of steps to nurture preterm and low-birth-weight babies.
This skin-to-skin method provides the baby with warmth and easy access to breastfeeding while promoting bonding, faster growth and weight gain.[1] Midwife Rose counseled Helena and her husband to continue kangaroo care at home and to come back to the dispensary every week for a check-up and to monitor progress. In six weeks, Neema (as the once tiny baby girl was named) doubled her weight. By the December holidays, a grinning, 4-month old, Neema weighed 7.2 kilograms (16 pounds), healthy and thriving after her premature birth.
When competent, caring midwives are in charge, more and smaller babies survive, even thrive, with a basic level of skilled care.
Reducing maternal and newborn deaths in rural Tanzania
Despite advances in maternal and newborn health over the past two decades, nearly 300,000 women across the world die every year from pregnancy and childbirth complications. Moreover, many children, like Helena’s, are born premature, the leading cause of death of children under 5.

In Tanzania, almost 20 women die every day due to childbirth-related complications, leaving families devastated and many children motherless. For every woman who dies, 20 or 30 suffer injuries, infections or disabilities.[1] The situation is worse in rural areas like Miswaki Village where competent health workers are either unavailable or ill-equipped and long-distances, impassable roads and poverty further limit access to quality care.
With support from the Canadian government, Jhpiego and its partners—Amref Health Africa, Tanzania Midwives Association and the Canadian Association of Midwives—joined with the Tanzanian government to carry out the More and Better Midwives for Rural Tanzania Project to improve the quality of care women and newborns receive.
“Walk in the shoes of that mother”
The More and Better Midwives project supported 20 health training institutions, including the Kisare Nursing School where Midwife Rose studied, to update the schools’ curriculum and faculty and prepare students to provide quality, respectful midwifery care when deployed. The project began in spring 2016 and ends this March.
“We teach our students to regard a pregnant woman or one who is in labor as if she was their mother or sister. ‘Walk in the shoes of that mother. Assume you are in her situation. Do what you are going to do next as you would have liked that done unto you by giving her appropriate quality care you would have demanded from a health provider,’” said Elijah Ernest, a midwife and senior tutor at Kisare Nursing School. “Today it is this mother. Tomorrow it can be you.”
The project’s focus is on competency-based, gender-sensitive learning where students participate in hands-on practice with life-size, anatomical models. It works to ensure equitable advancement and leadership opportunities for female and male midwives.
Another priority is developing empathy in health workers, a key factor in improving a client’s experience of pregnancy and childbirth care. The More and Better Midwives project has graduated 2,036 new nurse-midwives, equipping them with the clinical skills and confidence to assess, prevent and manage complications at birth in rural areas.
These are the same skills Midwife Rose recently exhibited at the Miswaki Dispensary. It was midday and the crush of clients had eased. Birds were chirping and a choir could be heard rehearsing at a nearby church when Rose’s mobile phone rang, its chirp signaling an urgent call.
“I am in pain. I cannot move. I cannot walk,” said the alarmed voice on the other end.
An urgent call
Rose immediately recognized the caller as Tatu Shabani, whom Rose had attended at the Miswaki antenatal clinic about a week before. Tatu, a 28-year-old mother of a 7-year-old girl, had a history of persistent high blood pressure, a condition that had resulted in the loss of her second pregnancy. Rose had advised Tatu and her husband Jumanne Ramadhani to plan for Tatu to deliver at Ndala Hospital, an advanced health facility some 90 kilometers away, to be certain of appropriate and timely care.
But Tatu’s onset of pain overtook the couple. Rose dispatched the local ambulance to retrieve her client.
“When she arrived . . . the blood pressure was dangerously high. We had to think fast and make a decision,” said Rose.
With Tatu’s cervix fully dilated, an indication that the baby was imminent, traveling to a faraway hospital was not possible.
Rose and her colleagues initiated the pre-eclampsia management protocol she learned through the More and Better Midwives project. They rushed Tatu to the one-bed labor room and followed the steps to successfully manage Tatu’s severe pre-eclampsia, a result of high blood pressure. The young midwife’s decision in this remote village saved Tatu and her new baby girl, who she named Pili.
Steadfast and with a smile, Midwife Rose delivers
A proud midwife who loves her job, Rose says she signed on at Miswaki Dispensary five months ago for one reason—to provide the best midwifery and safe motherhood care to her clients. “As a midwife, I feel so happy when I hear a mother appreciates my care and that it was the best care she ever received. My heart is overjoyed,” Rose said.
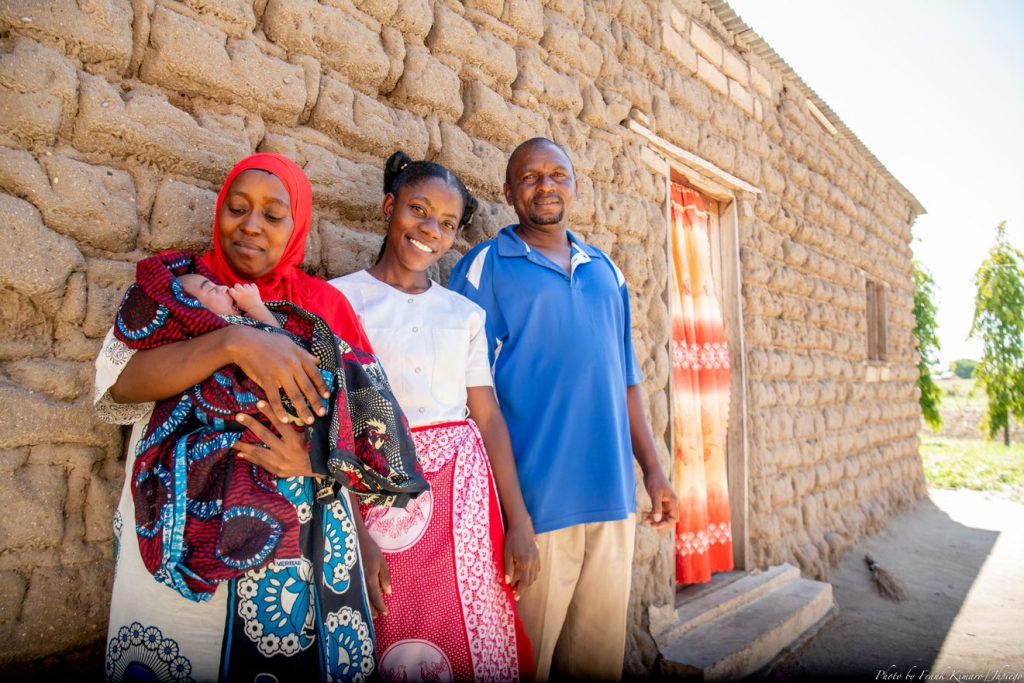
Upon her return to the health center, Helena Paschal showed off her baby daughter, Neema, who is the picture of health. After the close calls of her first two pregnancies, Helena and her husband, on the advice of Midwife Rose, have relocated to Miswaki Village to live near a health facility. “If it was not for Midwife Rose, I was going to lose my baby, again,” Helena said, cuddling her daughter.
She could have lost her life too. The family is taking no more chances.
With her client closer to health services, Midwife Rose is thinking ahead. “I want to go far,” she says. “I want to save more lives.”

Charles Wanga is the Communications Manager for the Africa Region. Frank Kimaro is a Communications Officer in Jhpiego’s Tanzania office.
[1] UNFPA. Transformative result: Ending preventable maternal deaths.



